Pathogenesis of Shoulder (Glenohumeral Joint) Osteoarthritis

Pathogenesis of Shoulder (Glenohumeral Joint) Osteoarthritis
‘You’re in pain because your joints are wearing away.’
You need to wear a sling to protect the joint! You need to stop doing all activities or else it’s going to wear away even more!
That’s not really the case.
There are many risk factors for shoulder osteoarthritis, including age, genetics (a positive family history increases risk), female gender, obesity, inflammation, injury (dislocation, fracture).1,2
Joint damage is either coming from specific factors with normal cartilage under mechanical loading (i.e. injury, fracture, joint instability) to abnormal cartilage under normal loading (i.e. age, genetics, sex, obesity, inflammation). These factors lead to a common biomechanical cascade leading to joint damage.6
On the extreme spectrum certain activities can increase the risk of shoulder arthritis. These include certain very strenuous occupations, such as heavy construction work and high end overhead sports, are also risk factors.1
However, these extreme working conditions like heavy construction and high level sports are the exception to the rule. The majority of the people won’t get to these extremes. Therefore, physical activity, in general, is not a risk factor for developing shoulder arthritis.
In reality, disease progression is, however, typically affected by a combination of genetic, behavioural and environmental factors.

Pathogenesis of OA: A continuum of proportional effect from specific factors.
Systemic & Non-Specific Risk Factors
By far, the principal risk factor in the development of shoulder arthritis is aging. Sounds pretty obvious right!? The scientific reason behind this simple principle is that chondrocyte density in the hyaline cartilage and responsiveness to growth factor slows down as we age. Less of the protective stuff leaves our joints vulnerable to damage.7
Genetics also plays a huge role in the development of arthritis. It’s estimated that 35% to 65% of arthritis is attributed to genetic influence.8
Obesity is also a known risk factor for hip and knee OA. This makes sense - they are weight bearing joints. Simple biomechanics. However, it’s also been associated with non-weight bearing joints. It’s been suggested that adipose tissue affects the endocrine function promoting low-grade inflammation that affects not only our arteries but also our joints.9
Local & Non-Specific Risk Factors
This category includes exercise and occupation.
We all know that a reasonable amount of joint loading is good for joint health. Adequate loading can maintain or even improve the biomechanical properties of healthy hyaline cartilage and subchondral bone.10
However, like anything, we get into trouble when there is too much or too little of something - in this case being joint loading.
On one end of the spectrum, insufficient stimulus through a sedentary lifestyle and muscle weakness that leads to abnormal joint motions propagates joint damage and wear.11
On the other end of the spectrum, excessive mechanical load poses a risk for increased joint surface wear. Heavy construction work and overhead sports are identified risk factors for glenohumeral osteoarthritis with elite tennis players showing glenohumeral joint osteoarthritis changes in their dominant shoulders.1,12 Other high-level athletes are at risk of developing glenohumeral joint osteoarthritis including weight lifters and throwing athletes such as baseball players.13
Interestingly, although high rates of shoulder pain are reported in wheelchair users, shoulder arthritis does not seem to be very prevalent in this patient population. This would suggest that simply mechanical stress from regular physical activity does not have a strong contribution to shoulder arthritis.14
Local & Specific Risk Factors
Glenohumeral instability, following both dislocation and instability surgery, can lead to arthritis. It’s reported that direct joint damage and altered biomechanics will lead to arthritis in as high as 56% to 68% of patients.15,16
Is it the instability episode or the surgery or both that causes the arthritis? The answer is that we don’t really know but they probably both contribute to the end result. We do know that patients with a single shoulder dislocation have a 10- to 20-fold increased risk of developing radiological GHOA compared to persons without acute shoulder injuries.17 We also know that recurrent dislocations, older age at primary dislocation, and greater trauma energy further increase the risk of GHOA development.15,16
Fractures can cause macroscopic articular cartilage damage which can lead to joint destruction. Posttraumatic osteoarthritis can come about from humeral head fractures as well as glenoid fracture. Also iatrogenic joint damage can occur from hardware penetration following surgical fracture fixations.
Rotator cuff arthropathy can come about from traumatic or degenerative rotator cuff tears. This eventually leads to erosion of the superior glenoid, resulting in acetabularization of the coracoacromial arch, and rounding off of the humeral greater tuberosity.18
Glenohumeral chondrolysis is a rare iatrogenic process resulting from intra-articular local anesthetic agents, bioabsorbable anchors, and thermal damage during arthroscopy.19
Scapular morphology is also associated with glenohumeral joint arthritis. These include the lateral extension of the acromion as well as glenoid inclination. These two measurements have been combined to give the critical shoulder angle (CSA). Normal values were between 30° and 35°. Both a shorter acromion and a greater inferior glenoid inclination (leading to a lower CSA) result in compressive forces by the deltoid muscle. Values of <30° being implicated in medially directed compressive force across the glenohumeral joint and may lead to excess loading and subsequent OA.20
Glenoid dysplasia, an anomaly of the scapula that is characterized by a bony deficiency of the posteroinferior glenoid and the adjacent scapular neck, caused by abnormal development of the two ossification centers in the glenoid, is a further risk factor for shoulder arthritis.21 You would think that this is a rare condition but it’s thought that it can be seen in 14% to 40% of shoulders.22
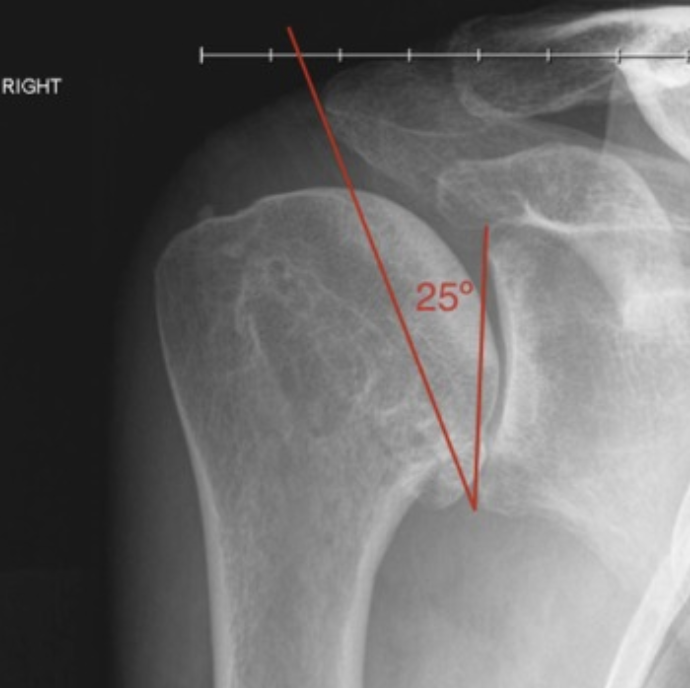
The critical shoulder angle of <30° being implicated in shoulder OA.26
Systemic & Specific Risk Factors
Inflammatory arthritis, such as rheumatoid, psoriatic, juvenile, spondyloarthropathies and systemic lupus erythematosus, are all autoimmune mediated diseases that can cause shoulder arthritis. Typically, the pain these patients experience likely relates to the inflammatory synovitis, rather than the joint destruction itself. Crystalline arthropathies, including gout and pseudogout, can also lead to shoulder arthritis.24
Avascular osteonecrosis (AVN) of the humeral head leads to bony collapse and loss of joint congruity. It’s fairly common accounting for approximately 5% of all shoulder arthritis. The more common causes of AVN stem from factors such as trauma, corticosteroid use and alcoholism.23
Neuropathic arthropathy also known as charcot arthropathy, is another rare degenerative disorder characterized by rapid destruction of the joint with extensive involvement of the bone and soft tissue. Cervical syringomyelia accounts for 75% of neuropathic shoulder arthropathy, while other causes of insensitivity, such as diabetes mellitus, chronic alcoholism, or end-stage renal disease, are less common.25
Shoulder Imaging
Imaging, Clinical Symptoms & Shoulder Arthritis
The link between radiological findings and the patients symptoms has been shown to be weak and these changes are very common in the asymptomatic population.4,15,32
Radiographs & Shoulder Arthritis
Loss of joint space, formation of osteophytes and deformation are common features of osteoarthritis. However, do bigger osteophytes lead to more pain? What about loss of joint space, does this lead to greater disability? Should all patients with severe glenohumeral degenerative joint disease receive a joint replacement?
Kicher et al.3 retrospectively examined 120 standardized X-rays of patients with advanced osteoarthritis of the shoulder. They looked at joint space and size of humeral head osteophytes.
As age increased, the joint space narrowed. However, joint space width was not correlated with size of a humeral head osteophyte. It was also not correlated with pain, active or passive range of motion.
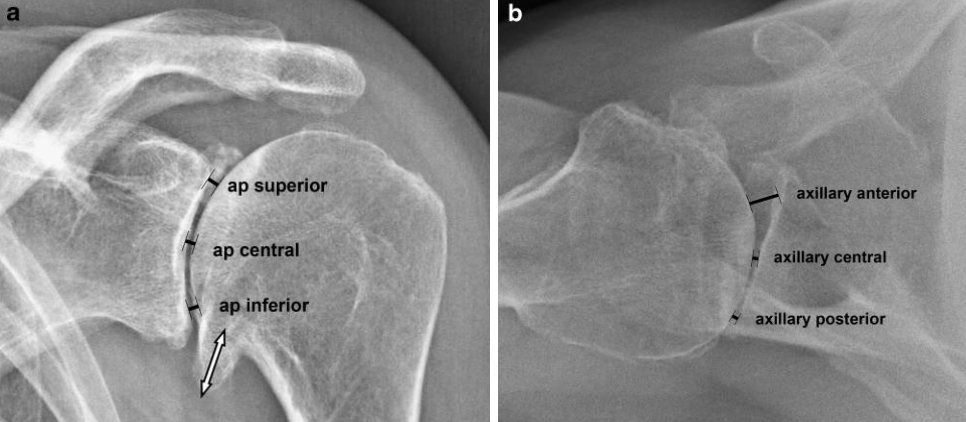
(a) True anteroposterior x-ray and (b) axillary view of a left shoulder with advanced osteoarthritis.3
MRI & Shoulder Arthritis
One high‐quality radiographic study looked at the prevalence of structural shoulder pathology using X-ray and MRI in three groups of older people: those with current shoulder pain, those with a previous history of shoulder pain and those with no history of shoulder pain.4
They found that shoulder pathology is apparent in both symptomatic and asymptomatic shoulders and clinical symptoms may not match radiological findings. With regards to arthritis they reported no relationship between acromioclavicular joint or glenohumeral joint osteoarthritis and pain.4
Another MRI study looked at 23 Ironman triathletes, seven asymptomatic, 16 symptomatic and a separate, non-triathlete group was evaluated specifically for AC joint marrow signal abnormalities.5

MRI findings on symptomatic and asymptomatic Ironman triathletes.5
Clinically Relevant Osteoarthritis
Joint Damage
We all know that we can diagnose arthritis on x-rays and when the patient has joint pain. Joint damage is caused by either abnormal mechanical stress on normal cartilage or normal stress on structurally weakened cartilage. These are on the opposite end of the spectrum. However joint damage does occur, once it’s started it propagates a cascade of biochemical events that further the wear and synovitis.
We tend to see focal or global cartilage loss and subsequent subchondral bony sclerosis are most pronounced in the upper two-thirds of the humeral head. This area is in contact with the glenoid between 60 and 100 degrees of abduction.27
Joint Pain
The synovium and subchondral bone are richly innervated. It’s these structures that are the source of nociceptive stimuli. It’s these structures that likely cause pain.28
Increased pressure on the subchondral bone, from altered biomechanics or cartilage damage, can lead to the pain symptoms patients experience on a day-to-day basis.
In addition to the local painful structures around the joint, an individual’s pain sensation is modified by local and central pain pathways as well as psychosocial and financial factors.28
That’s why we’ll see in a clinic a patient that has pre-existing depression or anxiety with much higher pain levels than you’d expect for that particular patient’s objective radiological findings of joint damage. Other common factors that can lead to this discordance between subjective and objective symptoms includes coping mechanisms and the patient's education level. It’s also been well documented that workers’ compensation cases and other legal cases (i.e. motor vehicle accident claims), where compensation claims are commonly related to poorer outcomes.29,30,31
Clinically Relevant Osteoarthritis
We can have patients with joint pain but no arthritis. We can have patients with radiological osteoarthritis but no pain. In the end, a patient with both joint pain and radiological osteoarthritis are the only patients that should be treated for their clinically relevant arthritis.
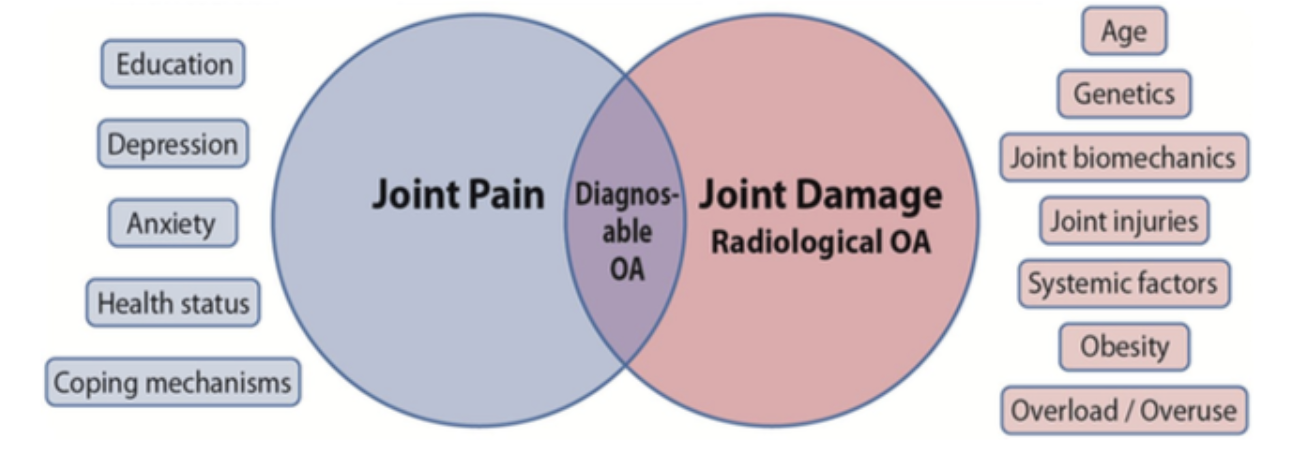
Only patients with joint pain and radiological changes that overlap have clinically relevant osteoarthritis.6
References
- Millett PJ, Gobezie R, Boykin RE. Shoulder osteoarthritis: diagnosis and management. Am Fam Physician. 2008 Sep 1;78(5):605-11. PMID: 18788237.
- Felson DT. An update on the pathogenesis and epidemiology of osteoarthritis. Radiol Clin North Am. 2004 Jan;42(1):1-9, v. doi: 10.1016/S0033-8389(03)00161-1. PMID: 15049520.
- Kircher J, Morhard M, Magosch P, Ebinger N, Lichtenberg S, Habermeyer P. How much are radiological parameters related to clinical symptoms and function in osteoarthritis of the shoulder?. Int Orthop. 2010;34(5):677-681. doi:10.1007/s00264-009-0846-6
- Gill TK, Shanahan EM, Allison D, Alcorn D, Hill CL. Prevalence of abnormalities on shoulder MRI in symptomatic and asymptomatic older adults. Int J Rheum Dis. 2014 Nov;17(8):863-71. doi: 10.1111/1756-185X.12476. Epub 2014 Oct 8. PMID: 25294682.
- Reuter RM, Hiller WD, Ainge GR, Brown DW, Dierenfield L, Shellock FG, Crues JV 3rd. Ironman triathletes: MRI assessment of the shoulder. Skeletal Radiol. 2008 Aug;37(8):737-41. doi: 10.1007/s00256-008-0516-6. Epub 2008 Jun 10. PMID: 18542952.
- Ibounig T, Simons T, Launonen A, Paavola M. Glenohumeral Osteoarthritis: An Overview of Etiology and Diagnostics. Scand J Surg. 2020 Jul 14:1457496920935018. doi: 10.1177/1457496920935018. Epub ahead of print. PMID: 32662351.
- Martin JA, Buckwalter JA. The role of chondrocyte senescence in the pathogenesis of osteoarthritis and in limiting cartilage repair. J Bone Joint Surg Am. 2003;85-A Suppl 2:106-10. doi: 10.2106/00004623-200300002-00014. PMID: 12721352.
- Fernández-Moreno M, Rego I, Carreira-Garcia V, Blanco FJ. Genetics in osteoarthritis. Curr Genomics. 2008;9(8):542-547. doi:10.2174/138920208786847953
- Tu C, He J, Wu B, Wang W, Li Z. An extensive review regarding the adipokines in the pathogenesis and progression of osteoarthritis. Cytokine. 2019 Jan;113:1-12. doi: 10.1016/j.cyto.2018.06.019. Epub 2018 Jun 28. PMID: 30539776.
- Sanchez-Adams J, Leddy HA, McNulty AL, O'Conor CJ, Guilak F. The mechanobiology of articular cartilage: bearing the burden of osteoarthritis. Curr Rheumatol Rep. 2014 Oct;16(10):451. doi: 10.1007/s11926-014-0451-6. PMID: 25182679; PMCID: PMC4682660.
- Slemenda C, Brandt KD, Heilman DK, Mazzuca S, Braunstein EM, Katz BP, Wolinsky FD. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997 Jul 15;127(2):97-104. doi: 10.7326/0003-4819-127-2-199707150-00001. PMID: 9230035.
- Maquirriain J, Ghisi JP, Amato S. Is tennis a predisposing factor for degenerative shoulder disease? A controlled study in former elite players. Br J Sports Med. 2006 May;40(5):447-50. doi: 10.1136/bjsm.2005.023382. PMID: 16632577; PMCID: PMC2653874.
- Carfagno DG, Ellenbecker TS. Osteoarthritis of the glenohumeral joint: nonsurgical treatment options. Phys Sportsmed. 2002 Apr;30(4):19-30. doi: 10.3810/psm.2002.04.253. PMID: 20086520.
- Bossuyt FM, Arnet U, Brinkhof MWG, Eriks-Hoogland I, Lay V, Müller R, Sunnåker M, Hinrichs T; SwiSCI study group. Shoulder pain in the Swiss spinal cord injury community: prevalence and associated factors. Disabil Rehabil. 2018 Apr;40(7):798-805. doi: 10.1080/09638288.2016.1276974. Epub 2017 Jan 13. PMID: 28084832.
- Kavaja L, Pajarinen J, Sinisaari I, Savolainen V, Björkenheim JM, Haapamäki V, Paavola M. Arthrosis of glenohumeral joint after arthroscopic Bankart repair: a long-term follow-up of 13 years. J Shoulder Elbow Surg. 2012 Mar;21(3):350-5. doi: 10.1016/j.jse.2011.04.023. Epub 2011 Aug 3. PMID: 21813296.
- Hovelius L, Saeboe M. Neer Award 2008: Arthropathy after primary anterior shoulder dislocation--223 shoulders prospectively followed up for twenty-five years. J Shoulder Elbow Surg. 2009 May-Jun;18(3):339-47. doi: 10.1016/j.jse.2008.11.004. Epub 2009 Feb 28. PMID: 19254851.
- Marx RG, McCarty EC, Montemurno TD, Altchek DW, Craig EV, Warren RF. Development of arthrosis following dislocation of the shoulder: a case-control study. J Shoulder Elbow Surg. 2002 Jan-Feb;11(1):1-5. doi: 10.1067/mse.2002.119388. PMID: 11845141.
- Ecklund KJ, Lee TQ, Tibone J, Gupta R. Rotator cuff tear arthropathy. J Am Acad Orthop Surg. 2007 Jun;15(6):340-9. doi: 10.5435/00124635-200706000-00003. PMID: 17548883.
- Yeh PC, Kharrazi FD. Postarthroscopic glenohumeral chondrolysis. J Am Acad Orthop Surg. 2012 Feb;20(2):102-12. doi: 10.5435/JAAOS-20-02-102. PMID: 22302448.
- Moor BK, Bouaicha S, Rothenfluh DA et al: Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? A radiological study of the critical shoulder angle. Bone Joint J 2013; 95-B(7): 935–941.
- Allen B, Schoch B, Sperling JW, Cofield RH. Shoulder arthroplasty for osteoarthritis secondary to glenoid dysplasia: an update. J Shoulder Elbow Surg. 2014 Feb;23(2):214-20. doi: 10.1016/j.jse.2013.05.012. Epub 2013 Aug 9. PMID: 23937928.
- Harper KW, Helms CA, Haystead CM, Higgins LD. Glenoid dysplasia: incidence and association with posterior labral tears as evaluated on MRI. AJR Am J Roentgenol. 2005 Mar;184(3):984-8. doi: 10.2214/ajr.184.3.01840984. PMID: 15728629.
- Hasan SS, Romeo AA. Nontraumatic osteonecrosis of the humeral head. J Shoulder Elbow Surg. 2002 May-Jun;11(3):281-98. doi: 10.1067/mse.2002.124347. PMID: 12070505.
- Parsons IM 4th, Weldon EJ 3rd, Titelman RM, Smith KL. Glenohumeral arthritis and its management. Phys Med Rehabil Clin N Am. 2004 May;15(2):447-74. doi: 10.1016/j.pmr.2003.12.001. PMID: 15145425.
- Snoddy MC, Lee DH, Kuhn JE. Charcot shoulder and elbow: a review of the literature and update on treatment. J Shoulder Elbow Surg. 2017 Mar;26(3):544-552. doi: 10.1016/j.jse.2016.10.015. Epub 2017 Jan 19. PMID: 28111181.
- Mantell MT, Nelson R, Lowe JT, Endrizzi DP, Jawa A. Critical shoulder angle is associated with full-thickness rotator cuff tears in patients with glenohumeral osteoarthritis. J Shoulder Elbow Surg. 2017 Dec;26(12):e376-e381. doi: 10.1016/j.jse.2017.05.020. Epub 2017 Jul 20. PMID: 28735840.
- De Palma AF: Surgery of the Shoulder, 3rd ed. Lippincott, Philadelphia, PA, 1983, pp. 211–241.
- Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. Lancet. 2005 Mar 12-18;365(9463):965-73. doi: 10.1016/S0140-6736(05)71086-2. PMID: 15766999.
- Loughlin J. Genetic contribution to osteoarthritis development: current state of evidence. Curr Opin Rheumatol. 2015 May;27(3):284-8. doi: 10.1097/BOR.0000000000000171. PMID: 25775188; PMCID: PMC4423655.
- Chapman K, Valdes AM. Genetic factors in OA pathogenesis. Bone. 2012 Aug;51(2):258-64. doi: 10.1016/j.bone.2011.11.026. Epub 2011 Dec 8. PMID: 22178404.
- Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015 Apr;23(4):507-15. doi: 10.1016/j.joca.2014.11.019. Epub 2014 Nov 29. PMID: 25447976.
- Kobayashi T, Takagishi K, Shitara H, Ichinose T, Shimoyama D, Yamamoto A, Osawa T, Tajika T. Prevalence of and risk factors for shoulder osteoarthritis in Japanese middle-aged and elderly populations. J Shoulder Elbow Surg. 2014 May;23(5):613-9. doi: 10.1016/j.jse.2013.11.031. Epub 2014 Feb 20. PMID: 24561177.
