Classifications of Shoulder Instability

The Classifications of Shoulder Instability
Shoulder instability, particularly glenohumeral instability, is a frequent and well-documented issue in sports medicine. Shoulder instability occurs when the humeral head partially or completely dislocates from the glenoid fossa, often due to trauma, repetitive strain, or ligamentous laxity, leading to pain, weakness, and a sensation of the shoulder "slipping".
Classification systems help guide treatment:
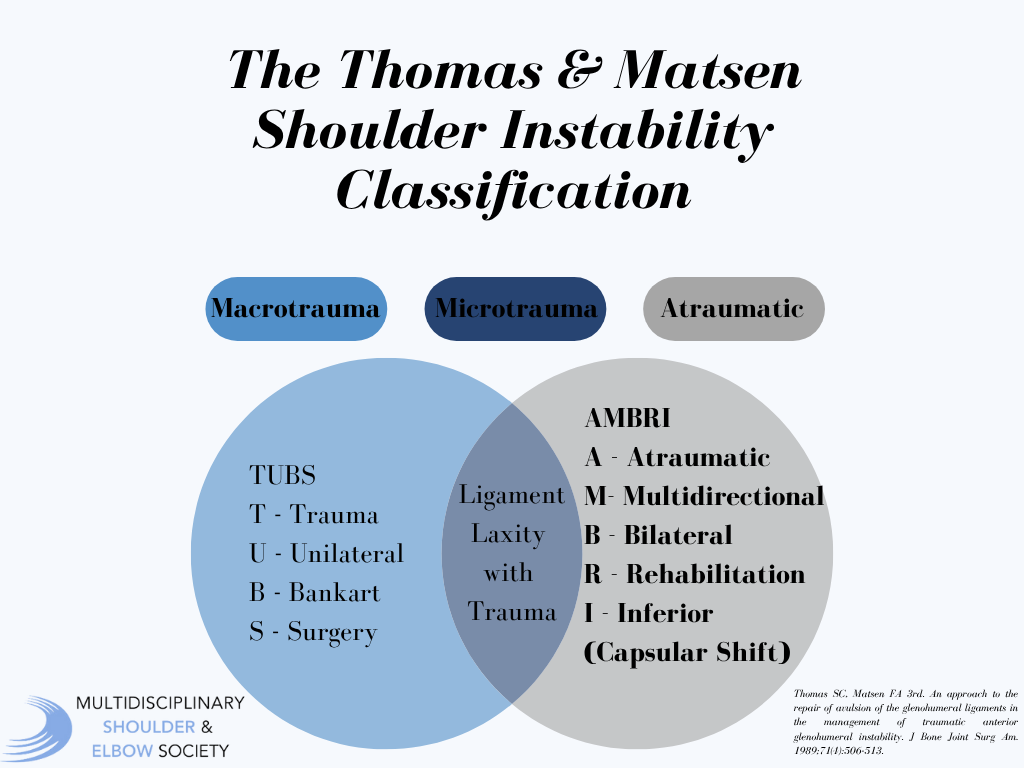
The Thomas & Matsen system categorizes instability into TUBS (Traumatic, Unidirectional, Bankart lesion, requiring Surgery) and AMBRI (Atraumatic, Multidirectional, Bilateral, Rehabilitation, Inferior capsular shift).
The Stanmore classification identifies a continuum of instability types: Polar I (traumatic structural), Polar II (atraumatic structural), and Polar III (neuromuscular/muscle-patterning), acknowledging shifts between categories over time.
Gerber’s system classifies instability as static (structural abnormalities), dynamic (trauma-induced with capsulolabral damage), or voluntary (intentional dislocation), emphasizing the role of hyperlaxity and structural integrity.
These frameworks inform decisions between surgical intervention and conservative management.
Pathology of Shoulder Instability
Three primary components confer stability to the shoulder joint:1
- The conformity of the humeral head on the smaller glenoid cavity, which is deepened by the labrum.
- The negative pressure (suction effect) within the joint capsule, reliant on capsule integrity.
- The compressive action of surrounding muscles, including the rotator cuff, which stabilize the humeral head against the glenoid.
Interestingly, the absence of one or more of these factors does not always result in instability. Instability may arise from:1
- Structural deficiencies (traumatic or atraumatic)
- Impaired muscular activity and coordination
- Forces exceeding the joint’s capacity to maintain integrity
Additional considerations include:1
- Time: Instability severity and type can evolve, as initial traumatic dislocations may be followed by subsequent, less traumatic events.
- Hyperlaxity: This is a structural abnormality, often due to altered collagen composition, leading to increased joint laxity. Hyperlaxity differs from instability but can contribute to its development.
Classification Systems
Thomas & Matsen Classification2
The Matsen system divides patients into two groups:
- TUBS: Traumatic, Unilateral, Bankart lesion, Surgery. These patients typically have a traumatic injury with identifiable structural lesions (e.g., Bankart or Hill-Sachs lesions) and often require surgical intervention.
- AMBRI: Atraumatic, Multidirectional, Bilateral, Rehabilitation, Inferior Capsular Shift. These patients have capsular laxity (not precisely defined) and are managed primarily with physiotherapy, with surgery reserved for refractory cases.
Limitations of this system include its failure to address hyperlaxity, the coexistence of traumatic and atraumatic features, and changes in pathology over time.
Gerber Classification3
To address these gaps, Gerber introduced a six-type system:
- Locked/Chronic Dislocation
- Unidirectional Instability (with/without hyperlaxity)
- Multidirectional Instability (with/without hyperlaxity)
- Voluntary Instability
This classification recognizes voluntary control of dislocation and allows for the description of evolving pathology over time. It also acknowledges the possibility of multiple coexisting pathologies, which can complicate treatment.
Muscle Patterning Disorders4
Research at the Royal National Orthopaedic Hospital (Stanmore) highlighted the significance of muscle patterning disorders in instability. Dynamic electromyography in over 1,000 patients revealed that about 50% had abnormal muscle patterning, with higher rates in posterior (85%) and inferior (100%) instability. Patients with muscle patterning disorders have poorer surgical outcomes, making identification crucial for successful management.
Treatment of Muscle Patterning Disorders
Conventional physiotherapy is less effective for pure muscle patterning disorders. However, specialized interventions—such as biofeedback and targeted muscle retraining—have shown better outcomes. For example, biofeedback programs have demonstrated significant improvements in function, though complete shoulder stabilization is achieved in only a subset of patients.
The Stanmore (Bayley’s Triangle) Classification5
The Stanmore classification, developed at Stanmore, integrates previous systems and expands them to include:
- Traumatic causes
- Atraumatic structural causes (including hyperlaxity)
- Muscle patterning disorders
Patients can be positioned anywhere within a triangular model to reflect the relative contributions of each factor, and the model can be projected into three dimensions to account for changes over time.

Conclusion
A comprehensive classification system should facilitate optimal treatment by accurately identifying the underlying causes of instability. The Stanmore classification currently offers the most inclusive framework, accommodating both simple and complex cases, including those involving muscle patterning disorders. This system guides clinicians in selecting appropriate interventions, whether specialized physiotherapy or surgical repair.
References
- Cuéllar R, Ruiz-Ibán MA, Cuéllar A. Anatomy and Biomechanics of the Unstable Shoulder. Open Orthop J. 2017 Aug 31;11:919-933. doi: 10.2174/1874325001711010919. PMID: 28979600; PMCID: PMC5611901.
- Thomas SC, Matsen FA 3rd. An approach to the repair of avulsion of the glenohumeral ligaments in the management of traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 1989;71(4):506-513.
- Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res. 2002;(400):65-76. doi:10.1097/00003086-200207000-00009
- The Role of Dynamic Electromyography in Muscle Patterning Instability. British Elbow & Shoulder Society Annual Meeting Edinburgh 2006
- The Classification of Shoulder Instability. New Light Through Old Windows. Lewis A, Kitamura T, Bayley JIL, Current Orthopaedics 2004 18:97-108
